How Bad Is My Ulcerative Colitis?
According to the Truelove-Witts classification of disease severity, my ulcerative colitis is mild. My partial Mayo Score of 0 indicates disease remission.
My gastroenterologist diagnosed me with ulcerative colitis in March 2018, i.e., 27 months ago.
The mention of “ulcerative colitis” to the average layperson rarely elicits a reaction, presumably because they don’t know what the term means (nor do I expect them to). Therefore, I often refer to my ulcerative colitis (UC) as a “lifelong gut problem” when speaking to laypersons.
In contrast, when I tell healthcare professionals, especially medical doctors, that I have UC, their reaction is very different – usually, some combination of shock, empathy, and concern – probably because of a presumption my UC is severe or life-threatening. In my line of work, I run into many healthcare professionals, which means I often have to clarify any misconceptions about UC and describe how the disease affects me.
In reality, the biggest issue with my UC is taking mesalazine (mesalamine; 5-aminosalicylate (5-ASA); brand name: Salofalk) three times a day, particularly remembering to take my mid-day dose. I have my mid-day dose with my afternoon tea to solve this problem. Swallowing two Salofalk tablets (total: 1 gram) just before I have German sourdough rye bread and a cup of coffee late afternoon is now part of my daily routine. My UC doesn’t otherwise affect my everyday life.
Nevertheless, it might be prudent to review my UC against established criteria.
Several indexes for assessing disease activity in UC are available, e.g.:
- Truelove and Witts’ severity index
- Mayo Score
- Seo index
- Rachmilewitz index
- Simple Clinical Colitis Activity index
- PRO2
There is broad agreement among most of these clinical activity indexes, so it probably doesn’t matter which one we select.
I’ll first describe my disease in its current state, using the parameters used in these indexes, and other ones, as a guide.
Clinical Symptoms and Signs
Stool frequency
I have very regular bowel movements – once a day, usually late morning, after breakfast. I don’t remember having the urgency of defecation or loss of control in the last two years.
Stool consistency
My stools have consistently been Type 4 on the Bristol stool scale, i.e., normal. I rarely have constipation, but if I do, it is almost always because of inadequate fluid intake or a recent change in diet. I haven’t had a single episode of diarrhea since March 2018.
Presence of blood
I have had no rectal bleeding since I started taking mesalazine in March 2018, i.e., over two years ago.
Abdominal pain
I experience colicky abdominal pain about once a week, either in the right lower quadrant or the left side of my abdomen (but never in both locations simultaneously). The pain begins around bedtime and is usually associated with bloating. In virtually all instances, the aggravating factor is a slight deviation from my usual diet in the preceding 12 hours. Over a few hours, the pain goes away. I suspect this abdominal pain is because of irritable bowel syndrome rather than UC.
Fatigue
Fatigue is a symptom I often experience and to varying degrees. The fatigue can be pretty debilitating on rare occasions. Episodes of fatigue can last from several hours to a few consecutive days, but never more than a week at a time. There are no obvious precipitating or exacerbating factors I have identified. Through experience, I have found that regular aerobic exercise, such as rowing, running, and cycling, helps to reduce the frequency of episodes and mitigate their severity. Exercise is like medicine for me – I just do it whether I’m in the mood for it. Other than my scheduled rest days, there are relatively few instances I don’t do my daily workout:
- I am feeling too fatigued (the most typical reason by far);
- Work or work-related travel does not allow it (sort of hard to work out if you’re sitting in an airport/plane/train/bus/cab for hours on end, checking into a hotel past midnight and expecting to give a talk or attend a business meeting a few hours later);
- I am at a location where any form of workout, even running, is physically impossible; or
- Something I have prioritized over my workout, which I cannot deal with at a time before or after the period I would otherwise do my workout, and I cannot (reasonably) fit my workout at any other time during the day. This situation is infrequent – it happens fewer than five times in a calendar year.
My fatigue has a few potential causes: UC, irritable bowel syndrome, the medications I’m taking for these two conditions, or something else.
Fever
I have not had a fever for years, certainly not since my UC diagnosis.
Heart rate
My resting heart rate is between 45 and 50 beats per minute, probably physiological bradycardia (slower than the average heart rate) induced by endurance exercise training. In recent memory, I’ve not had tachycardia (faster than standard heart rate) at rest.
Blood Tests
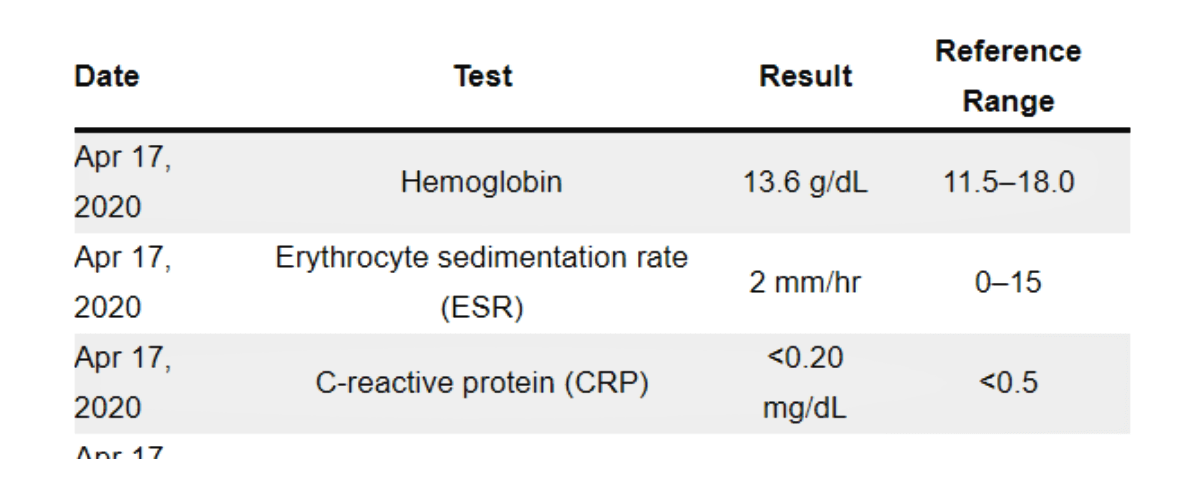
The four relevant blood tests are: hemoglobin (looking for anemia), erythrocyte sedimentation rate (ESR, a marker of inflammation) and C-reactive protein (CRP, another inflammatory marker), and serum albumin. As part of a battery of tests, these tests were last on April 17, 2020, i.e., about two months ago.
| Date | Test | Result | Reference Range |
|---|---|---|---|
| Apr 17, 2020 | Hemoglobin | 13.6 g/dL | 11.5–18.0 |
| Apr 17, 2020 | Erythrocyte sedimentation rate (ESR) | 2 mm/hr | 0–15 |
| Apr 17, 2020 | C-reactive protein (CRP) | <0.20 mg/dL | <0.5 |
| Apr 17, 2020 | Albumin | 40 g/L | 37–55 |
Colonoscopy
My last colonoscopy was in February 2018. I am due for a repeat colonoscopy in a couple of months – this should tell us if the distal proctitis, seen on colonoscopy two years ago, has resolved.
Truelove and Witts’ Severity Index
According to this index, one can classify the severity of UC as mild, moderate, or severe. My UC disease severity is mild based on Truelove and Witts’ severity index.
| Parameter | Mild |
|---|---|
| Number of bowel movements per day | Fewer than 4 |
| Blood in stools | No more than small amounts of blood |
| Pyrexia (temperature >37.8°C) | No |
| Pulse rate >90 beats per minute | No |
| Anemia (<10g/dL) | No |
| Erythrocyte sedimentation rate (ESR) (mm/hr) | 30 or below |
Partial Mayo Score for Ulcerative Colitis Activity
The partial Mayo score uses the three non-invasive components of the full Mayo Score, i.e., stool frequency, rectal bleeding, and physician’s global assessment, and excludes the score for the endoscopic findings.
| Parameter | Clinical evaluation | Score |
|---|---|---|
| Stool frequency | Normal | 0 |
| Rectal bleeding | None | 0 |
| Physician’s global assessment | Normal | 0 |
| Partial Mayo Score | 0 |
My partial Mayo score is 0. A score of <2, i.e., 0 or 1, is interpreted as “Remission.”
Conclusion
Fortunately, my UC has been clinically quiescent, i.e., in remission, since my UC diagnosis in March 2018. I took both oral and rectal mesalazine to induce remission. I stopped taking the mesalazine suppositories after three months, but I’m still on oral mesalazine at a dose of 3 grams per day.