My Laboratory Fasting Blood Glucose Test Result Is Above Normal. Am I Prediabetic?
Over the past nine months, three laboratory-based fasting blood glucose tests yielded measurements at or above the American Diabetes Association’s cut-point for prediabetes. However, some factors point against a diagnosis of prediabetes, and there is at least one alternative explanation for my abnormally high fasting blood glucose levels.
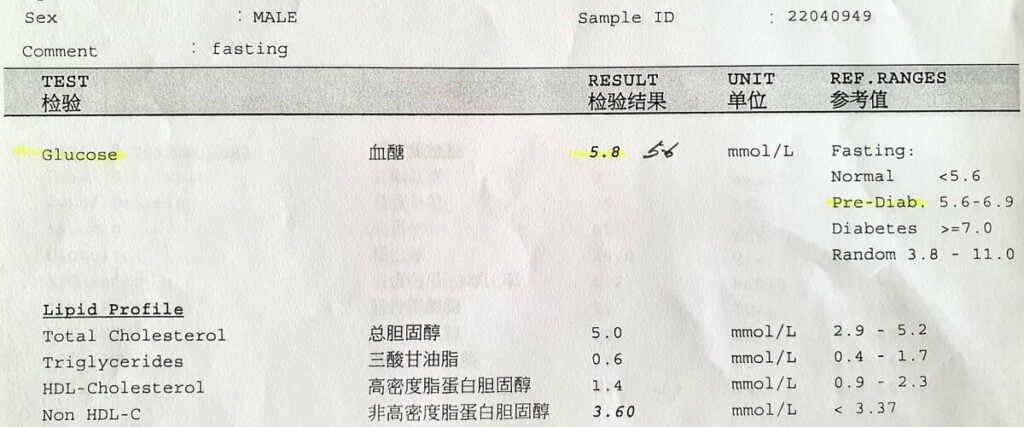
On March 29, 2022, my fasting blood glucose level (sugar level) was 5.8 mmol/L or 104.5 mg/dL. This level fell in the “prediabetes” category according to the laboratory reference ranges.
Two fasting blood glucose levels, taken about 6 and 9 months earlier, were 5.6 mmol/L, also in the prediabetes range.
On April 17, 2020, my fasting blood glucose was 5.1 mmol/L.
Fasting blood glucose levels (mmol/L), July 6, 2021–March 29, 2022.
On the last three occasions when my fasting glucose was 5.6 mmol/L or higher, the result surprised me because a person with my body habitus, diet, and physical activity should not have a fasting glucose level of 5.6 mmol/L, let alone 5.8 mmol/L. Considering my family history of type 2 diabetes (my father has the condition), age (I’m over 45), and Southeast Asia ancestry, I could not believe it.
Clinical acumen, intuition, plain common sense – call it whatever you will, I suspected something was amiss.
What Is Prediabetes?
Prediabetes is a metabolic disorder characterized by elevated glucose levels but not high enough to be diabetic. It is a risk factor for several conditions including diabetes mellitus (usually Type 2 diabetes), nephropathy and chronic kidney disease, neuropathies and diabetic retinopathy, macrovascular disease, and major adverse cardiac events (MACE).
Prediabetes is a reversible condition.
Tests to Diagnose Prediabetes
Our blood glucose level (blood sugar level) is like our blood pressure; it fluctuates throughout the day, depending on a variety of factors:
- Food – type, quantity, the timing of consumption
- Physical activity – intensity, duration, aerobic training
- Medical conditions
- Medications
- Stress
- State of hydration – dehydration can cause a rise in blood glucose
- Sleep – quantity, quality
- Age
- Time of the day
We usually diagnose prediabetes by measuring:
- Fasting blood glucose (aka fasting blood sugar or fasting plasma glucose);
- Two-hour post-load plasma glucose; or
- Glycated hemoglobin (HbA1c).
For each of the three tests above, various professional bodies, such as the World Health Organization (WHO), American Diabetes Association (ADA), and International Expert Committee (IEC), have determined three different ranges of values that are:
- Normal
- Prediabetic
- Diabetic
We may diagnose a person as prediabetic if they meet one or more of the following conditions:
- Impaired Fasting Glucose
- Impaired Glucose Tolerance
- Elevated HbA1c
Impaired Fasting Glucose
A person has impaired fasting glucose if their blood glucose level is above the normal range but below the level to diagnose diabetes, having fasted for at least 8 hours. Hence, if someone’s fasting glucose level is in the range between the upper limit of normal and the threshold value (cut-point) for diagnosing diabetes, we will deem them as having impaired fasting glucose and, therefore, prediabetes.
WHO 1 1. World Health Organization & International Diabetes Federation. (2006). Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. World Health Organization. https://apps.who.int/iris/handle/10665/43588 × and ADA 2 2. American Diabetes Association; 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care 1 January 2021; 44 (Supplement_1): S15–S33. https://doi.org/10.2337/dc21-S002 × have different normal and prediabetic ranges of fasting glucose:
| Professional Body | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| WHO | < 6.1 mmol/L | 6.1–6.9 mmol/L | ≥ 7.0 mmol/L |
| < 110 mg/dL | 110–125 mg/dL | ≥ 126 mg/dL | |
| ADA | < 5.6 mmol/L | 5.6–6.9 mmol/L | ≥ 7.0 mmol/L |
| < 100 mg/dL | 100–125mg/dL | ≥ 126 mg/dL |
The last three measurements of my fasting blood glucose met the ADA criterion for diagnosing prediabetes based on fasting blood glucose. Only one ADA criterion is required to define prediabetes.
Impaired Glucose Tolerance
Both WHO and ADA define impaired glucose tolerance as a glucose level of 7.8–11.0 mmol/L (140–199 mg/dL) two hours after a 75-g oral glucose tolerance test.
I have not had a glucose tolerance test.
Elevated HbA1c
HbA1c represents the average blood glucose level over two to three months.
The following table shows the HbA1c-based definitions of prediabetes by ADA and IEC.
| Professional Body | HbA1c to Define Prediabetes |
|---|---|
| ADA | 5.7–6.4% |
| 39–47 mmol/mol | |
| IEC | 6.0–6.4% |
| 42–47 mmol/mol |
My HbA1c on October 5, 2021, was 5.0%, well within normal limits.
Why I Don’t Believe I’m Prediabetic
Despite the three consecutive fasting blood glucose results showing prediabetes (if we use the ADA cut-points), I was and still am unconvinced I’m prediabetic. I explain why below.
I Had Minimized My Risk of Developing Prediabetes
The three risk factors for developing prediabetes I’ve identified are all non-modifiable:
- Age over 45 years
- Having a first-degree relative with type 2 diabetes mellitus
- Southeast Asia background
On the flip side, I have done my best to minimize the risk factors associated with prediabetes, e.g.
- I am not overweight – my BMI is 22.6, i.e., below the “at-risk” value of 23
- I am physically active – I exercise at least 45 minutes almost every day
- My diet is healthy, balanced, and modest
- I have a normal blood pressure
- The levels of HDL cholesterol and triglycerides are within the normal range
In my assessment, the pretest probability of me having prediabetes in March 2022 was low, i.e., less than 10%.
Fasting Blood Glucose Unresponsive to Weight Loss, Regular Exercise, and Healthy Diet
After I learned my fasting blood glucose level was 5.6 mmol/L on July 6, 2021, I shed 8.5% of my body weight over three months through regular exercise and dietary control. But this did not get meaningful results – my fasting blood glucose was again 5.6 mmol/L on October 5, 2021.
A similar thing happened at my last appointment. This time, I had lost 850 grams of body weight – the law of diminishing returns was in play – but my fasting blood glucose was paradoxically higher.
In nine months, I had lowered my weight by 7.15 kg, or 9.6% of my body weight, but my fasting blood glucose had risen from 5.6 mmol/L to 5.8 mmol/L.
The exercise, diet, and weight loss should have, in theory, improved my insulin sensitivity and reduced my blood glucose level measured on March 29. The level did not go down; it went up instead, making little sense.
If someone had newly diagnosed me with diabetes or prediabetes, I know they would have told me to change my lifestyle. But what if the lifestyle changes had preceded the diagnosis by nine months?
Alternative Explanations for the Rise in My Fasting Blood Glucose
Is it possible that the three fasting blood glucose levels were high despite me being normoglycemic (not prediabetic and not diabetic)?
I can think of two realistic conditions that would have led to this situation:
- Transient elevation of my fasting blood glucose because of the stress of being in a clinical environment (“white coat hyperglycemia”)
- Transient elevation of my fasting blood glucose because of prednisolone, a glucocorticoid medication (steroid hyperglycemia)
Although laboratory error is something to consider, I don’t think this is a viable explanation. I am confident the laboratory performs the fasting blood glucose test with high reliability and precision.
White-Coat Hyperglycemia
White-coat hyperglycemia refers to elevated blood glucose associated with an impending visit to a doctor’s office or medical procedure.
I have diagnosed white-coat hypertension in a few of my patients, but I’ve never come across a patient with white-coat hyperglycemia.
Two consecutive in-laboratory results, six months apart, had not shown improvement in my fasting blood sugar despite recommended lifestyle changes and weight loss, which was a sign I needed to check the level in a non-clinical environment.
Fortunately, the procedure was simple.
I got my hands on a Contour Next One glucose meter, or glucometer, by Ascensia Diabetes Care, previously known as Bayer Diabetes Care, and an Accu-Chek FastClix lancing device.

The first home measurement of my blood glucose, having fasted for over 11 hours on April 12, 2022, was 5.2 mmol/L, or 93.7 mg/dL.

To confirm my fasting blood glucose was normal, I performed another check on the glucometer two days later, i.e., April 14. The result was the same as on April 12 – 5.2 mmol/L.

The value of 5.2 mmol/L obtained from my home blood glucose monitor, on two occasions two days apart (April 12 and 14), was significantly lower than that from the laboratory-based test (5.8 mmol/L on March 29).
It seems improbable that the Contour Next One would give grossly inaccurate measurements. The device meets the minimum accuracy requirements of the ISO 15197:2013 standard. These requirements are:
- 95% of the measured glucose values within either:
- ±15 mg/dL (±0.83 mmol/L) of the average measured values of the reference measurement procedure at glucose concentrations <100 mg/dL (<5.55 mmol/L); or
- ±15% at glucose concentrations ≥100 mg/dL (≥5.55 mmol/L).
- 99% of individual glucose measured values need to fall within zones A and B of the Consensus Error Grid (CEG) for type 1 diabetes.
Nevertheless, “+/- 15%” of the laboratory-based glucose measurement still means a wide range. For example, if the laboratory-based result, assumed to be the actual value, was 5.8 mmol/L, any home glucometer reading between 5.0 and 6.6 will still be considered accurate!
The fasting blood glucose reading of 5.2 mmol/L on my home glucometer also seems more consistent with the HbA1c concentration of 5.0% on October 5, 2021.
I have made the following conclusions:
- I am probably not prediabetic.
- There is a moderate probability I suffered white-coat hyperglycemia on my July 7, 2021 clinic appointment and since then.
Steroid Hyperglycemia
While preparing to write this post, I realized there was another explanation for the high in-laboratory fasting blood glucose measurements on the days of my last three clinic appointments: a medication called prednisolone.
Use of Prednisolone to Treat Allergic Rhinitis
For years, I have used prednisolone to treat allergic rhinitis. Though it may seem to be an unconventional treatment choice, a single dose of prednisolone for an episode works better for me than antihistamines or nasal steroid sprays.
A side-effect of prednisolone is insulin resistance and high blood glucose levels.
Temporal Relationship Between One-Off Prednisolone Doses and Fasting Blood Glucose Measurements
Below are some relevant dates on which I took prednisolone before a fasting blood glucose test.
| Date Prednisolone Taken | Prednisolone dose | Date of test | Days before test | Fasting blood glucose (mmol/L) |
|---|---|---|---|---|
| 06/13/2021 | 5 mg | 07/06/2021 | 22 | 5.6 (lab) |
| 09/15/2021 | 10 mg | 10/05/2021 | 20 | 5.6 (lab) |
| 03/23/2022 | 5 mg | 03/29/2022 | 6 | 5.8 (lab) |
| 04/09/2022 | 5 mg | 04/12/2022 | 3 | 5.2 (home) |
| 04/09/2022 | 5 mg | 04/14/2022 | 5 | 5.2 (home) |
As you can see from the table, my fasting blood glucose measurements do not correlate with the prednisolone dose or with the time I took the drug relative to the test. Therefore, prednisolone was unlikely to have had a significant effect on my fasting blood glucose levels.
Game Plan
Regardless of whether I’m genuinely prediabetic, I should aim to lower my overall blood glucose. I’ll use the Model for Improvement, developed by Associates in Process Improvement, which I am very familiar with, to achieve this.
In the Model for Improvement, we answer three fundamental questions:
- What are we trying to accomplish?
- How will we know that a change is an improvement?
- What change can we make that will result in improvement?
What are we trying to accomplish?
My goal is a laboratory-based fasting blood glucose level of 5.5 mmol/L at my next gastroenterology clinic appointment, scheduled at the end of September.
How will we know that a change is an improvement?
We will know if a specific change is an improvement if my blood glucose monitor readings are lower. For example, after regular calisthenics for a month, a value of 5.1 mmol/L or lower on the glucometer will tell me the calisthenics helped improve my glycemic control.
What change can we make that will result in improvement?
I have a few changes lined up:
- Return to light running, rowing and cycling as much as my sciatic symptoms allow
- Do calisthenics training to build muscle mass (increasing insulin sensitivity)
- Introduce bitter melon, also known as bitter gourd, to my diet
- Extend my daily fast to 18 hours, i.e., an 18:6 regimen
- Increase hours of sleep by an hour
- Meditate for 10 minutes a day
Applying the Plan-Do-Study-Act (PDSA) Cycle
Having answered the three questions of the Model for Improvement, I will apply the PDSA cycle.
I will test the changes in my plan in turn; I won’t be trying them simultaneously. By testing the changes one by one and observing the results after each test of change, I’ll be able to identify which changes helped and which didn’t.
Subsequently, I’ll act on what I learned from each test of change. For example, if 15–20 minutes of calisthenics per day helps, I might increase it to 30 minutes a day. If eating bitter melon twice a week doesn’t help, I might either eat it more frequently or discard the idea of eating it.
Assessing the Accuracy of My Glucometer
When I next have my fasting blood glucose tested in a laboratory, I’ll bring my glucometer along and use it to test my blood glucose level immediately after phlebotomy. I can then compare the reading on the glucose meter against the laboratory result and, in that way, evaluate the precision of the device.
Conclusion
Using the ADA cut-points, three consecutive fasting blood glucose tests in a laboratory showed levels consistent with prediabetes.
However, my apparent impaired fasting glucose did not improve after recommended lifestyle changes and almost 10% of weight loss.
Normal fasting blood glucose readings on my home glucometer suggest white coat hyperglycemia.
Regardless of whether I have prediabetes, it will be prudent to lower my overall blood glucose level by non-pharmacological means.
Reference(s)
- World Health Organization & International Diabetes Federation. (2006). Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. World Health Organization. https://apps.who.int/iris/handle/10665/43588 ↩
- American Diabetes Association; 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care 1 January 2021; 44 (Supplement_1): S15–S33. https://doi.org/10.2337/dc21-S002 ↩